SEPTEMBER 5, 2024. By Amrit Tiwana, Nicola Gale, and Sofia Bartlett.
People who experience criminalization, such as those who have been incarcerated, often struggle with unstable housing, or use drugs, are more likely to be affected by sexually transmitted and bloodborne infections (STBBIs) like HIV and hepatitis C. They face many barriers to getting treatment, including unstable living conditions, stigma, and poverty. Compared to people who aren’t criminalized, these groups have a much tougher time receiving the STBBI treatment they need.
The COVID-19 pandemic made these problems worse as many healthcare services quickly switched to virtual care. For people without reliable access to the internet or a phone, getting healthcare became almost impossible.
To reduce this gap and improve outcomes for those with STBBIs, the Test, Link, Call (TLC) Project has stepped in to support people who experience criminalization across British Columbia. By providing cell phones and peer support, the TLC Project is helping people access care for HIV, hepatitis B, and hepatitis C.
The Test, Link, Call Project
This peer-based project began in September 2021 and is a collaboration between the BC Centre for Disease Control (BCCDC), BC Mental Health & Substance Use Services, BC Hepatitis Network, and Unlocking the Gates (UTG) Services Society. Led by Dr. Sofia Bartlett (BCCDC), Deb Schmitz (BC Hepatitis Network), and Pam Young (UTG), the project aims to expand access to STBBI treatment for people who experience criminalization.

TLC Project Process
Participants in the TLC Project receive a free personal cell phone with a 6-month unlimited plan, are paired with a Peer Health Mentor, and get help scheduling appointments for STBBI care.
Peer Health Mentors are staff members from UTG, a peer-led program that connects individuals transitioning from corrections back into their communities with social and health services. UTG mentors have been trained in the “Peers in Practice: Hepatitis C Support” program by the BC Hepatitis Network, and many have also completed additional training offered by the BCCDC, including “Hepatitis C: The Basics Online Course”.
Recruitment posters are shared in common areas of shelters, drug detox and recovery houses, and other services. These posters include UTG contact information. Most participants enroll after contacting or speaking with a Peer Health Mentor, who explains the project details, eligibility criteria, and participant commitments. Healthcare providers can also refer patients directly to the project. To enroll, participants must agree to be tested for HIV, hepatitis B, or hepatitis C or already know their test results. If an infection is confirmed, the Peer Health Mentor or healthcare provider gives the person a phone and helps connect them to STBBI treatment through a network of care providers.
Each phone is pre-loaded with contact information and apps designed to support participants in accessing STBBI treatment, harm reduction, and overall wellbeing. The address book includes numbers for their healthcare provider, Peer Health Mentor, and BC Help 4 Hep (toll-free). Additionally, the phones come with preloaded apps including:
- LifeGuard
- The Brave app
- MediSafe (for medication tracking and reminders)
- BC Virtual Visit (telehealth app)
- BC Services Locator (health service locator app)
- I’m Ready (for HIV self-testing)

When participants receive their phones, Peer Health Mentors help them with the contact information and apps loaded on the device. The mentors also assist in making the first contact with healthcare providers and discuss participants preferred method of communication, call or text, and how often they’d like check-ins. After the 6-month period, they get to keep the phones, and can choose to transition to a prepaid plan. This personalized support helps ensure that participants are comfortable using their phones and connected to the care they need.
How Far We’ve Come
Since the launch in September 2021, the TLC Project has made remarkable progress in enhancing healthcare access for people who experience criminalization. As of March 2024, the initiative has enrolled 273 participants for hepatitis C care and 26 for HIV care. Most participants receiving hepatitis C treatment are men aged 40 to 59 who are either unstably housed or without a fixed address. Many have a recent history of injecting drug use, and more than half of these people are on opioid agonist therapy (OAT). Among HIV participants, most are men aged between 40 and 59 with an unknown housing status.
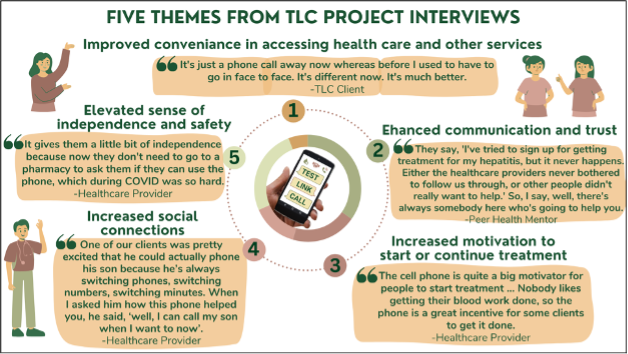
Communication barriers have been a significant challenge, primarily due to the lack of cell phones.
“Most of our patients don’t have cell phones, and if they do, rarely do they have minutes for us to get in contact with them.” Healthcare Provider
“So many clinics are not even offering in-person visits, so if you don’t have a phone, you can’t get healthcare.” Healthcare Provider
Providing cell phones through this initiative has greatly improved communication and motivation, appreciated by participants and providers.
“It’s made a great big difference considering I would never have been able to make any of my appointments without a phone.” Participant
“People get pretty excited about being able to contact me more often, you know, being able to contact their healthcare provider more often.” Healthcare Provider
The peer support is key to the project’s success.
“Having someone like me or a peer support worker who understands and is willing to just sit there through the process makes a big difference.” Peer Health Mentor
The phones have also provided access to other health and services.
“I got to use the phone to contact the optometrist and the dentist.” Participant
“I was able to use that phone and make phone calls, read messages, leave contact numbers for all the people that I was trying to contact for housing and for jobs. I want to get back in the working field.” Participant
The TLC Project has shown promising outcomes. Approximately 57% of participants enrolled for hepatitis C care have initiated curative treatment, compared to 52% among people who currently or previously use drugs in the 2020 BC Hepatitis Testers Cohort. This shows that the TLC Project is helping more people start curative treatment compared to standard care
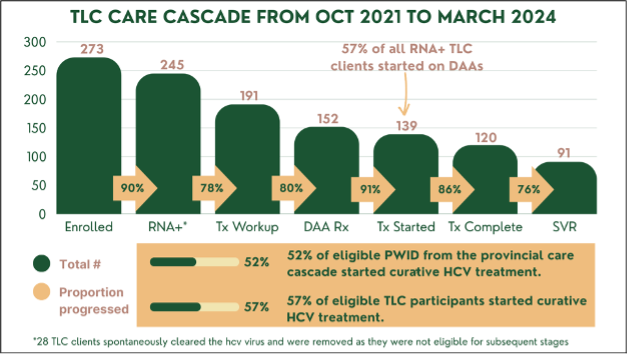
Abbreviations: PWID, people who inject drugs; SVR, SVR, sustained virologic response (i.e., viral cure); HCV, hepatitis C virus.
The TLC Project is an innovative initiative able to pave new paths to health equity for those experiencing criminalization. We look forward to expanding the project across British Columbia and recruiting people in need of syphilis treatment, with continued support from the Pacific Public Health Foundation.
Learn More
Visit Test, Link, Call Project | YouMatter and/or contact Dr. Sofia Bartlett at sofia.bartlett@bccdc.ca.
Acknowledgements
Thank you to all the TLC participants in this quality improvement project, especially those who joined interviews and shared their experiences. We also appreciate the support from these groups for their help with participant recruitment and engagement: Unlocking the Gates Services Society, Alliance Clinic Surrey, ASK Wellness Society, AVI, BCMHSUS Correctional Health Services, Carrier Sekani First Nation Family Services, Coolaid Clinic, Dr. John Farley, Dr. Peter Centre, Fraser Health (Positive Health Services & IHART), Kilala Lelum, North Island Positive Wellness, Northern Health (HIV/HCV SST), Providence Health (RAAC Clinic), Ribbon Community, Vancouver Infectious Diseases Clinic, Vancouver Urban Health Centre, and Vancouver Coastal Health (Primary Care Outreach, ACT, VGH ID Clinic). Your support has been vital. Thank you!
As originally seen on the Pacific Public Health Foundation’s blog posts.