By Stephanie Gin, Nurse Educator, Clinical Prevention Services, BC Centre for Disease Control
British Columbia (BC) is now the first province or territory in Canada to recommend one-time birth cohort screening for people born from 1945 to 1965. This update is included in recent revisions to the British Columbia Centre for Disease Control (BCCDC) Communicable Disease Control (CDC) Manual and Guidelines and Protocol Advisory Committee (GPAC) viral hepatitis testing guidelines.
Updates to the Guidelines and Protocol Advisory Committee (GPAC) Viral Hepatitis Testing Guideline
GPAC is an advisory committee to the Medical Services Commission that develops BC Guidelines. These are clinical practice guidelines and protocols that provide recommendations to BC practitioners (target audience is physicians, nurse practitioners and medical students) on delivering high quality, appropriate care to patients with specific clinical conditions or diseases. More information and a list of their guidelines can be found at BCGuidelines.ca.
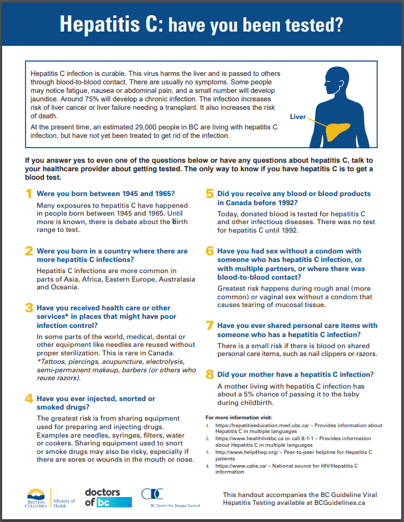
Currently, an estimated 28,600 diagnosed and undiagnosed people in BC are living with hepatitis C infection and remain untreated. The 1945 to 1965 birth cohort accounts for nearly 60% of positive hepatitis results in BC, and represents a key population that needs to be engaged into HCV care to reduce liver disease complications. Many people within this birth cohort are undiagnosed and have not received confirmatory HCV RNA testing.
Engagement sessions with patients helped to inform the development of an eight-question screening information sheet. This tool aims to help facilitate conversations between healthcare providers and patients in a non-stigmatizing and non-judgmental way.
Updates to the BCCDC Communicable Disease Control (CDC) Guidelines
The BCCDC CDC Guidelines assist healthcare providers working in public health and primary care with decision-making for specific situations and to support consistency of provincial public health practice.
Revisions to the BCCDC Hepatitis B, C and BBFE Management Guidelines were posted on April 13, 2021 (Admin Circular 2021:15). Most revisions relate to the Hepatitis C Guidelines and HCV RNA reflex testing that were implemented at the BCCDC Public Health Laboratory on January 13, 2020. Reflex testing was initiated because approximately 17% of people testing antibody positive in BC between 1990 and 2018 did not have a follow-up HCV RNA test to confirm a current infection. The ability to diagnose HCV infection from a single blood sample greatly improves patient care, by decreasing time to diagnoses and treatment, thereby decreasing potential loss to follow-up and related morbidity and mortality.
Below are highlights of the major revisions to the BCCDC CDC Guidelines:
Hepatitis C Guidelines
1) New Natural history of HCV infection figure
2) Refreshed Epidemiology section
3) Revised Hepatitis C Virus and Laboratory Information, reflecting recommendations made in CanHepC’s Blueprint to Inform Hepatitis C Elimination Efforts in Canada, and the GPAC Viral Hepatitis Testing Guideline:
– Clinical scenarios added where consideration of HCV testing is recommended.
– Disproportionately affected population groups experiencing higher rates of HCV infection in BC include:
- Born between 1945-1965, likely due to past acquisition risks (e.g., past IDU, healthcare received in countries where infection control practices were not followed or blood supply tested)
- Persons who have ever been incarcerated, where lack of access to harm reduction supplies leads to sharing of needles and unsterile tattooing practices
- Born or lived in regions where HCV is endemic
- Indigenous peoples, where health inequities contribute to national rates that are 4.7 times higher than non-indigenous populations
– Likelihood of transmission and activities associated with acquisition of HCV infection table refreshed (formerly “Risk factors for HCV Infection”), including:
- Injection drug use (IDU): approximately 85% of new HCV infections in Canada are related to IDU
- Condomless sex with multiple partners where blood is exchanged. More frequently reported in gbMSM engaging in group sex with concurrent substance use (i.e., “party ‘n play” or “chemsex”)
4) Simplified Management of Mother and Neonate to Determine Vertical Transmission recommendations:
- Anti-HCV testing at 18 months.
- Infants testing anti-HCV reactive at 18 months, should:
- Be referred to a paediatric infectious disease specialist or hepatologist for further testing and care.
- Receive routine infant vaccines.
5) New appendices: Examples of Laboratory Results, Quick Reference HCV Treatment Guide for Healthcare Providers, and Case Studies.
Blood and Body Fluid Exposure (BBFE) Management Guidelines
- Revisions throughout, reflecting HCV RNA reflex testing
- Examples of how to fill out BCCDC PHL Laboratory Requisitions for non-occupational health exposures
For more information and to sign up for BCCDC CDC Guideline updates, please see the BCCDC website.
References
1. Bartlett SR, Yu A, Chapinal N, Rossi C, Butt Z, Wong S, et al. The population level care cascade for hepatitis C in British Columbia, Canada as of 2018: Impact of direct acting antivirals. Liver International: Official Journal Of The International Association For The Study Of The Liver. 2019;39(12):2261-72.
2. BCCDC. New lab process reduces time from hepatitis C testing to treatment in B.C. July 24, 2020 [Available from: http://www.bccdc.ca/about/news-stories/stories/2020/new-lab-process-reduces-time-from-hepatitis-c-testing-to-treatment-in-b-c.
3. Krajden M, Cook D, Janjua NZ. Contextualizing Canada’s hepatitis C virus epidemic. Canadian Liver Journal. 2018.
This blog was first published on the SmartSexResource website